ERCP is an important technology for the diagnosis and treatment of biliary and pancreatic diseases. Once it came out, it has provided many new ideas for the treatment of biliary and pancreatic diseases. It is not limited to "radiography". It has transformed from the original diagnostic technology to a new type. Treatment techniques include sphincterotomy, bile duct stone removal, bile drainage and other methods to treat bile and pancreatic system diseases.
The success rate of selective bile duct intubation for ERCP can reach over 90%, but there are still some cases where difficult biliary access causes selective bile duct intubation failure. According to the latest consensus on diagnosis and treatment of ERCP, difficult intubation can be defined as: the time for selective bile duct intubation of the main nipple of conventional ERCP is more than 10 minutes or the number of intubation attempts is more than 5 times. When performing ERCP, if bile duct intubation is difficult in some cases, effective strategies should be selected in time to improve the success rate of bile duct intubation. This article conducts a systematic review of several auxiliary intubation techniques used to solve difficult bile duct intubation, with a view to providing a theoretical basis for clinical endoscopists to choose a response strategy when faced with difficult bile duct intubation for ERCP.
I.Singleguidewire Technique,SGT
The SGT technique is to use a contrastcatheter to continue trying to intubate the bile duct after the guide wire enters the pancreatic duct. In the early days of the development of ERCP technology, SGT was a common method for difficult biliary intubation. Its advantage is that it is simple to operate, fixes the nipple, and can occupy the opening of the pancreatic duct, making it easier to find the opening of the bile duct.
There are reports in theliterature that after conventional intubation fails, choosing SGT-assisted intubation can successfully complete bile duct intubation in about 70%-80% of cases. The report also pointed out that in cases of SGT failure, even the adjustment and application of double guidewire technology did not improve the success rate of bile duct intubation and did not reduce the incidence of post-ERCP pancreatitis (PEP).
Some studies have also shown that the success rate of SGT intubation is lower than that of double guidewire technology and transpancreatic papillary sphincterotomy technology. Compared with repeated attempts of SGT, early implementation of double guidewire technology or pre-incision technology can achieve better results.
Since the development of ERCP, a variety of new technologies have been developed for difficult intubation. Compared with single guidewire technology, the advantages are more obvious and the success rate is higher. Therefore, single guidewire technology is currently rarely used clinically.
II.Double-guide wire technique,DGT
DGT can be called the pancreatic duct guide wire occupation method, which is to leave the guide wire entering the pancreatic duct to trace and occupy it, and then the second guide wire can be re-applied above the pancreatic duct guide wire. Selective bile duct intubation.
The advantages of this approach are:
(1) With the assistance of a guidewire, the bile duct opening is easier to find, making bile duct intubation smoother;
(2) The guide wire can fixthe nipple;
(3) Under the guidance of the pancreatic duct guidewire, repeated visualization of the pancreatic duct can be avoided, thereby reducing the stimulation of the pancreatic duct caused by repeated intubation.
Dumonceau et al. noticed that a guidewire anda contrast catheter can be inserted into the biopsy hole at the same time, and then reported a successful case of the pancreatic duct guidewire occupying method, and concluded that the guidewire occupying the pancreatic duct method is successful for bile duct intubation. rate has a positive impact.
A study on DGT by Liu Deren et al. found that after DGT was performed on patients with difficult ERCP bile duct intubation, the intubation success rate reached 95.65%, which was significantly higher than the 59.09% success rate of conventional intubation.
A prospective study by Wang Fuquan et al. pointed out that when DGT was applied to patients with difficult ERCP bile duct intubation in the experimental group, the intubation success rate was as high as 96.0%.
The above studies show that the application of DGT to patients with difficult bile duct intubation for ERCP can effectively improve the success rate of bile duct intubation.
The shortcomings of DGT mainly include the following two points:
(1) The pancreatic guidewire maybe lost during bile duct intubation, or the second guidewire may enter the pancreatic duct again;
(2) This method is not suitable for cases such as pancreatic head cancer, pancreatic duct tortuosity, and pancreatic fission.
From the perspective of PEP incidence, the PEP incidence of DGT is lower than that of conventional bile duct intubation. A prospective study pointed out that the incidence of PEP after DGT was only 2.38% in ERCP patients with difficult bile duct intubation. Some literature points out that although DGT has a higher success rate of bile duct intubation, the incidence of post-DGT pancreatitis is still higher compared to other remedial measures, because the DGT operation may cause damage to the pancreatic duct and its opening. Despite this, consensus at home and abroad still points out that in cases of difficult bile duct intubation, when intubation is difficult and the pancreatic duct is repeatedly misentered, DGT is the first choice because DGT technology has relatively less difficulty in operation, and relatively easy to control.It is widely used in selective difficult intubation.
III.Wire guide cannulation-pan-creatic stent,WGC-P5
WGC-PS can also be called thepancreatic duct stent occupation method. This method is to place the pancreatic duct stent with the guidewire that mistakenly enters the pancreatic duct, then pull out the guidewire and perform bile duct cannulation above the stent.
A study by Hakuta et al. showed that in addition to improving the overall intubation success rate by guiding intubation, WGC-PS can also protect the opening of the pancreatic duct and significantly reduce the occurrence of PEP.
A study on WGC-PS by Zou Chuanxin et al. pointed out that the success rate of difficult intubation using the temporary pancreatic duct stent occupation method reached 97.67%, and the incidence of PEP was significantly reduced.
One study found that when a pancreatic duct stent is correctly placed, the chance of severe postoperative pancreatitis in difficult intubation cases is significantly reduced.
This method still has some shortcomings. For example, the pancreatic duct stent inserted during the ERCP operation may be displaced; if the stent needs to be placed for a long time after ERCP, there will be a high chance of stent blockage and duct obstruction. Injury and other problemslead to an increase in the incidence of PEP. Already, institutions have begun to study temporary pancreatic duct stents that can spontaneously move out of the pancreatic duct. The purpose is to use pancreatic duct stents to prevent PEP. In addition to significantly reducing the incidence of PEP accidents, such stents can also avoid other operations to remove the stent and reduce the burden on patients. Although studies have shown that temporary pancreatic duct stents have a positive effect in reducing PEP, their clinical application still has major limitations. For example, in patients with thin pancreatic ducts and many branches, it is difficult to insert a pancreatic duct stent. The difficulty will be greatly increased, and this operation requires a high professional level of endoscopists. It is also worth noting that the pancreatic duct stent placed should not be too long in the duodenal lumen. An excessively long stent may cause duodenal perforation. Therefore, the choice of pancreatic duct stent occupation method still needs to be treated with caution.
IV.Trans-pancreatocsphincterotomy,TPS
TPS technology is generally used after the guide wire enters the pancreatic duct by mistake. The septum in the middle of the pancreatic duct is incised along the directionof the pancreatic duct guide wire from 11 o'clock to 12 o'clock, and then the tube is inserted in the direction of the bile duct until the guide wire enters the bile duct.
A study by Dai Xin et al. compared TPS and two other auxiliary intubation technologies. It can be seen that the success rate of TPS technology is very high, reaching 96.74%, but it does not show outstanding results compared with the other two auxiliary intubation technologies. The advantages.
It has been reported that the characteristics of TPS technology include the following points:
(1) The incision is small for the pancreaticobiliary septum;
(2) The incidence of postoperative complications is low;
(3) The selection of the cutting direction is easy to control;
(4) This method can be used for patients with repeated pancreatic duct intubation or nipples within the diverticulum.
Many studies have pointed out that TPS can not only effectively improve the success rate of difficult bile duct intubation, but also does not increase the incidence of complications after ERCP. Some scholars suggest that if pancreatic duct intubation or small duodenal papilla occurs repeatedly, TPS should be considered first. However, when applying TPS, attention should be paid to the possibility of pancreatic duct stenosis and recurrence of pancreatitis, which are possible long-term risks of TPS.
V.Precut Sphincterotomy,PST
The PST technique uses the papillary arcuate band as the upper limit of the pre-incision and the 1-2 o'clock direction as the boundary to open the duodenal papilla sphincter to find the opening of the bile and pancreatic duct. Here PST specifically refers to the standard nipple sphincter pre-incision technique using an arcuate knife. As a strategy to deal with difficult bile duct intubation for ERCP, PST technology has been widely considered to be the first choice for difficult intubation. Endoscopic nipple sphincter pre-incision refers to the endoscopic incision of the papilla surface mucosa and a small amount of sphincter muscle through an incision knife to find the opening of the bile duct, and then use a guidewire or catheter to intubate the bile duct.
A domestic study showed that the success rate of PST is as high as 89.66%, which is not significantly different from DGT and TPS. However, the incidence of PEP in PST is significantly higher than that of DGT and TPS.
Currently, the decision to use this technology depends on a variety of factors. For example, one report stated that PST is best used in cases where the duodenal papilla is abnormal or distorted, such as duodenal stenosis or malignancy.
In addition, compared with other coping strategies, PST has a higher incidence of complications such as PEP, and the operation requirements are high, so this operation is best performed by experienced endoscopists.
VI.Needle-knife Papillotomy,NKP
NKP is a needle-knife-assisted intubation technique. When intubation is difficult, a needle-knife can be used to incise part of the papilla or sphincter from the opening of the duodenal papilla in the direction of 11-12 o'clock, and then use a guidewire or catheter to Selective insertion into the common bile duct. As a coping strategy for difficult bile duct intubation, NKP can effectively improve the success rate of difficult bile duct intubation. In the past, it was generally believed that NKP would increase the incidence of PEP in recent years. In recent years, many retrospective analysis reports have pointed out that NKP does not increase the risk of postoperative complications. It is worth noting that if NKP is performed in the early stage of difficult intubation, it will be of great help to improve the success rate of intubation. However, there is currently no consensus on when to apply NKP to achieve the best results. One study reported that the intubation rate of NKP applied during ERCP less than 20 minutes was significantly higher than that of NKP applied later than 20 minutes later.
Patients with difficult bile duct cannulation will benefit most from this technique if they have nipple bulges or significant bile duct dilation. In addition, there are reports that when encountering difficult intubation cases, the combined use of TPS and NKP has a higher success rate than applying alone. The disadvantage is that multiple incision techniques applied to the nipple will increase the occurrence of complications. Therefore, more research is needed to prove whether to choose early pre-incision to reduce the occurrence of complications or to combine multiple remedial measures to improve the success rate of difficult intubation.
VII.Needle-knife Fistulotomy,NKE
The NKF technique refers to using a needle knife to pierce the mucosa about 5mm above the nipple, using mixed current to incise layer by layer in the direction of 11 o'clock until the orifice-like structure or bile overflow is found, and then using a guide wire to detect the outflow of bile and incisionof the tissue. Selective bile duct intubation was performed on the jaundice site. NKF surgery cuts above the nipple opening. Due to the existence of the bile duct sinus, it significantly reduces thermal damage and mechanical damage to the opening of the pancreatic duct, which can reduce the incidence of PEP.
A study by Jin et al. pointed outthat the success rate of NK tube intubation can reach 96.3%, and there is no postoperative PEP. In addition, the success rate of NKF in stone removal is as high as 92.7%. Therefore, this study recommends NKF as the first choice for common bile duct stone removal. . Compared with conventional papillomyotomy, NKF operation risks are still higher, and it is prone to complications such as perforation and bleeding, and it requires high operating level of endoscopists. The correct window opening point, appropriate depth, and precise technique all need to be gradually learned. master.
Compared with other pre-incision methods, NKF is a more convenient method with a higher success rate. However, this method requires long-term practice and continuous accumulation by the operator to be competent, so this method is not suitable for beginners.
VIII.Repeat-ERCP
As mentioned above, there aremany ways to deal with difficult intubation. However, there is no guarantee of 100% success. Relevant literature has pointed out that when bile duct intubation is difficult in some cases, long-term and multiple intubation or the thermal penetration effect of pre-cut can lead to duodenal papilla edema. If the operation continues, not only will the bile duct intubation be unsuccessful, but the chance of complications will also increase. If the above situation occurs, you can consider terminating the current ERCP operation first and perform a second ERCP at an optional time. After the papilloedema disappears, the ERCP operation will be easier to achieve successful intubation.
Donnellan et al. performed a second ERCP operation on 51 patients whose ERCP failed after needle-knife preincision, and 35 cases were successful, and the incidence of complications did not increase.
Kim et al. performed a second ERCP operation on 69 patients who failed ERCP after needle-knife pre-incision, and 53 cases were successful, with a success rate of 76.8%. The remaining unsuccessful cases also underwent a third ERCP operation, with a success rate of 79.7%. , and multiple operations did not increase the occurrence of complications.
Yu Li et al. performed elective secondary ERCP on 70 patients who failed ERCP after needle-knife pre-incision, and 50 cases were successful. The overall success rate (first ERCP + secondary ERCP) increased to 90.6%, and the incidence of complications did not increase significantly. . Although reports have proven the effectiveness of secondary ERCP, the interval between two ERCP operations should not be too long, and in some special cases, delayed biliary drainage may aggravate the condition.
IX.Endoscopicultrasound-guided biliary drainage,EUS-BD
EUS-BD is an invasive procedure that uses a puncture needle to puncture the gallbladder from the stomach or duodenum lumen under ultrasound guidance, enter the duodenum through the duodenal papilla, and then perform biliary intubation. This technique includes both intrahepatic and extrahepatic approaches.
A retrospective study reported that the success rate of EUS-BD reached 82%, and the incidence of postoperative complications was only 13%. In a comparative study, EUS-BD compared with pre-incision technology, its intubation success rate was higher, reaching 98.3%, which was significantly higher than the 90.3% of pre-incision. However, so far, compared with other technologies, there is still a lack of research on the application of EUS for difficult ERCP intubation. There is insufficient data to prove the effectiveness of EUS-guided bile duct puncture technology for difficult ERCP intubation. Some studies have shown that it has reduced The role of postoperative PEP is not convincing.
X.Percutaneous transhepatic cholangial drainage,PTCD
PTCD is another invasive examination technique that can be used in combination with ERCP for difficult bile duct intubation, especially in cases of malignant biliary obstruction. This technique uses a puncture needle to percutaneously enter the bile duct, puncture the bile duct through the papilla, and then intubate the bile duct retrogradely through a reserved guidewire. One study analyzed 47 patients with difficult bile duct intubation who underwent PTCD technique, and the success rate reached 94%.
A study by Yang et al. pointed out that the application of EUS-BD is obviously limited when it comes to hilar stenosis and the need to puncture the right intrahepatic bile duct, while PTCD has the advantages of conforming to the bile duct axis and being more flexible in guiding devices. Bile duct intubation should be used in such patients.
PTCD is a difficult operation that requires long-term systematic training and the completion of a sufficient number of cases. It is difficult for novices to complete this operation. PTCD is not only difficult to operate, but the guidewire may also damage the bile duct during advancement.
Although the above methods can significantly improve the success rate of difficult bile duct intubation, the choice needs to be comprehensively considered. When performing ERCP, SGT, DGT, WGC-PS and other techniques can be considered; if the above techniques fail, senior and experienced endoscopists can perform pre-incision techniques, such as TPS, NKP, NKF, etc.; if still If selective bile duct intubation cannot be completed, elective secondary ERCP can be selected; if none of the above techniques can solve the problem of difficult intubation, invasive operations such as EUS-BD and PTCD can be tried to solve the problem, and surgical treatment can be selected if necessary.
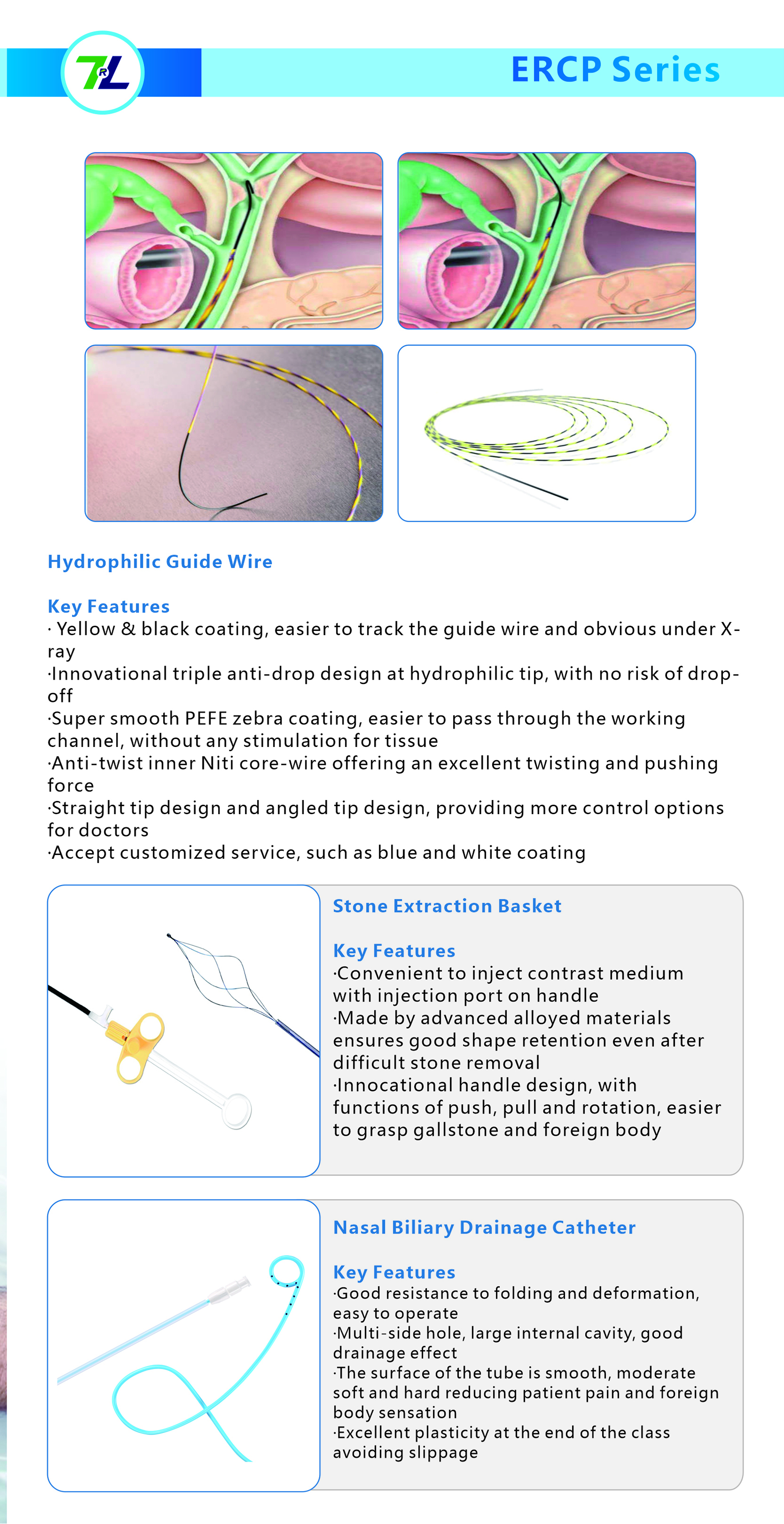
We, Jiangxi Zhuoruihua Medical Instrument Co.,Ltd., is a manufacturer in China specializing in the endoscopic consumables, such as biopsy forceps, hemoclip, polyp snare, sclerotherapy needle, spray catheter, cytology brushes, guidewire, stone retrieval basket, nasal biliary drainage catheter etc. which are widely used in EMR, ESD, ERCP. Our products are CE certified, and our plants are ISO certified. Our goods have been exported to Europe, North America, Middle East and part of Asia, and widely obtains the customer of the recognition and praise!
Post time: Jan-31-2024